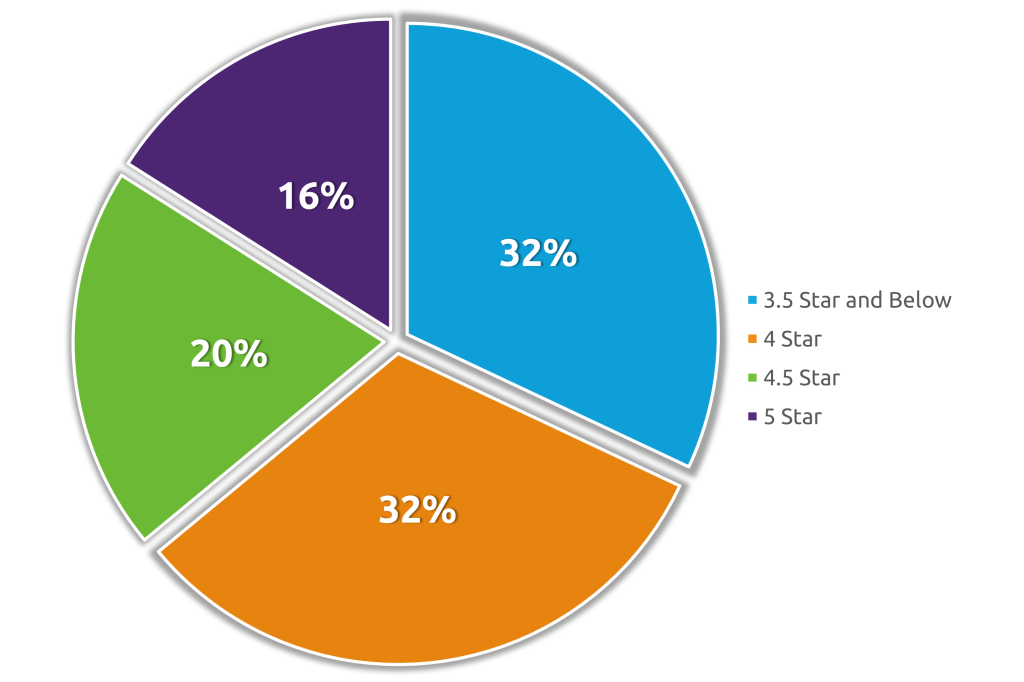
ATLANTA, GA, UNITED STATES - As an evidence-based partner, Curant Health leverages a proprietary approach to patient care that moves Star Ratings for health plan clients. Based on The Centers for Medicare and Medicaid (CMS) standards, health plans are given a Star Rating based on 5 measures: health management programs, chronic disease management, member satisfaction, pharmacy services, and customer service. Health plans are scored from a 1-star to 5-star scale, and a 5-star rating is defined as an excellent performance in the measure groups.[1] According to CMS, 33% of the Star measures consist of adherence to diabetic, hypertensive, and cholesterol medications, which is defined as a proportion of days covered (PDC) of 80% or greater.[1] In 2022, there were 471 health plans assigned a Star Rating.[2] As shown below, 84% of the health plans have room for measurable improvements in their Star Ratings.
To illustrate what successful partnership looks like, Curant Health provides member care for regional health plan partners. Using Curant Health’s data solutions and proprietary care models, Curant Health was able to successfully exceed CMS standards for regional health plans regarding medication adherence.
Care Management is a clinician-administered care model that utilizes a multidisciplinary clinical team to support members throughout their journey to improve health outcomes. Medication Management is a supplemental option focusing on complimentary specialty pharmacy service that includes a dedicated care coordinator, home medication delivery, and novel adherence packaging. In 2022, approximately 93% of members across regional health plans achieved a PDC of 80% or greater when receiving Care Management and Medication Management services from Curant Health.
Curant Health continues to prioritize member-centered care and has proven its proprietary approach to adherence. Their clinician-based interventions and pharmacy services can contribute to positive health outcomes and potential cost savings for health plans and their members. When receiving Care Management services alone, 94% of members achieve a PDC of 80% or greater.
It is imperative for health plans to partner with proven solutions that achieve meaningful improvements to their Star Rating. Curant Health’s proprietary approach to specialized member care has demonstrated measurable improvements in Star Ratings, and their health plan clients have found true value in Curant Health’s solutions. In addition, Curant Health has shown that a dedicated and highly trained clinical team can positively impact overall health outcomes.
About Us
Curant Health is a national outcomes-based patient support organization that specializes in improving adherence for challenging populations by leveraging advanced technology solutions with dedicated expert clinicians to deliver exceptional patient and partner outcomes.
For over two decades, we have improved medication adherence and health plan quality scores while reducing Total Cost of Care through proprietary algorithms that identify, engage, and monitor members in complex care populations.
Our solutions for Employers and Health Plans include products focused on Total Cost of Care Reduction, Productivity Improvement, High Cost & Complex Care Monitoring, Stars Adherence Improvement, HEDIS Gap Closure and Medication Reconciliation Post-Discharge.
We would love to learn more about you and your organization. We are confident we can make a positive impact on the lives of your members and invite you to learn more about us at www.curanthealth.com/healthplans.
We look forward to connecting!
[1] Centers for Medicare and Medicaid Services (CMS). https://www.cms.gov/files/document/2022-medicare-star-ratings-fact-sheet.pdf
[2] Centers for Medicare and Medicaid Services (CMS). https://www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovGenIn/PerformanceData
